Yesterday, it was a month since Gabriel was discharged from hospital.
Every day, it grows.
He begins to grasp objects and roll over onto his stomach when lying down.
His emotions vary very quickly from a fit of nerves to a burst of laughter.
He’s also intelligent and knows his world.
In short, he’s a baby who’s growing up, and so much the better!
However, our main concern remains its lung.
La it’s 4:58 just had a colic, and was crying to death stopping breathing, it’s always creepy.
It is worth noting, however, that after several complaints, we succeeded in obtaining a more precise fluxometer (a device used to regulate the oxygen delivered to the nostrils), enabling the flow rate to be set between 0, 0.5 and 1 L/min.

I’d been asking for it for months and was told it didn’t exist.
I had to do my own research, find some on the Internet, and finally show them what was needed (a neonatal fluxometer).
Finally, they found a slightly better version, but still imperfect (it allows you to talk about 0.5 L but not 0.1 L).
A baby who stays too long with too much oxygen can develop a pathology called bronchopulmonary dysplasia. The health plan seems to ignore this, even though all the physiotherapists are telling us so. (surprise !!!!)
Thanks to this device, we’ve been able to gradually lower the oxygen, and today he’s down to 0.5 L/min, while maintaining a saturation level of > 95%, which is a good sign.
On the other hand, he’s still breathing heavily and with a draught, which indicates that he’s putting a lot of effort into breathing, as part of his lungs are no longer working.
He therefore consumes a lot of energy and gets hot very quickly, as if he were running all the time, in fact.
This is typical of bronchiolitis obliterans and a baby’s lack of diaphragm muscles.
In this article, I’ll try to give you an idea of the day’s program.
This program is repeated every day without interruption, with only minor variations.
Our days
We are available around Gabriel :
Johann: from 1:00 to 8:00, then from 12:00 to 17:00
Manuela: 8am to 12pm, then 5pm to 1am
During these hours we are available but not necessarily present with him. Why? Because we have to work.
I’ll come back to this notion of work later.
At the same time, we hire two 24-hour helpers, Gleive and Nadine, to keep us on course.
Without them, it would be impossible: Gabriel has to be constantly monitored to make sure he doesn’t pull out his tube, or that his oxygen doesn’t come out of his nose, or that the milk doesn’t fall too quickly into his stomach.
It’s costing us around R$9,000 a month, but the health plan hasn’t agreed to fund a caregiver, despite the seriousness of her condition.
And when one of them falls ill… everything stops (this week, it was both of them who were ill at the same time).
In this case, we sleep little, stay with Gabriel and just do what’s necessary during the day.
The nights
Gabriel usually sleeps from 8pm to 2.30am.
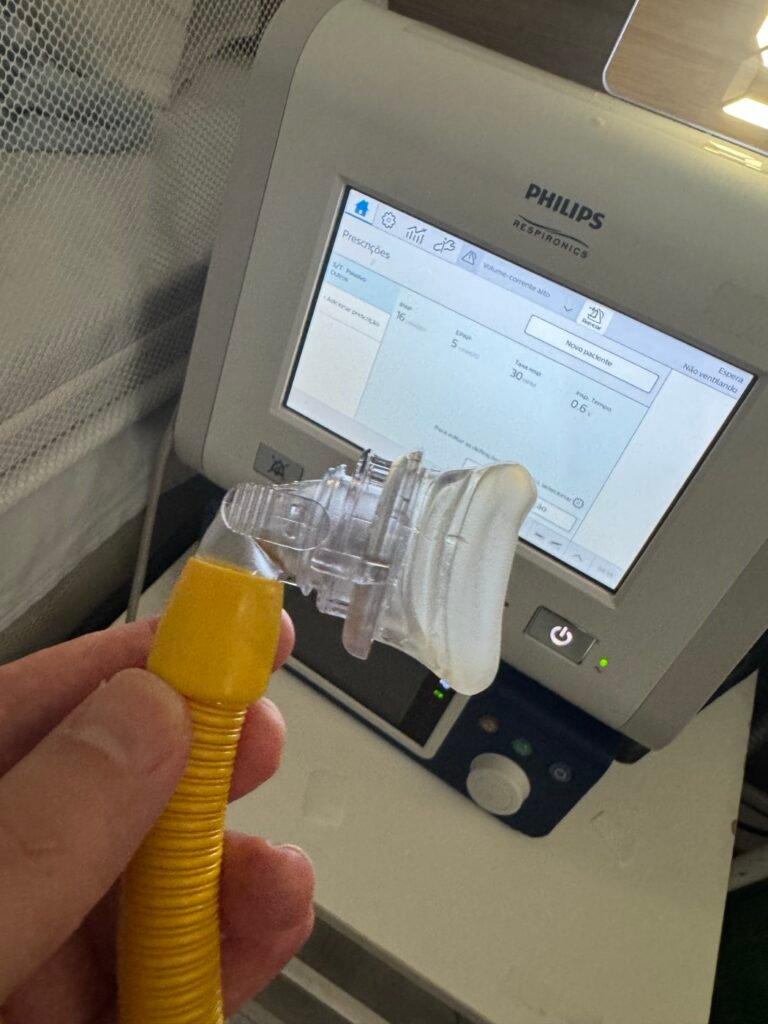
For the first part of the night, Manuela tries to get him to tolerate the NIV, a device that blows pressurized air into his lungs to help keep them open.
He hates having air blowing into his nose. So fitting him with a mask that presses on his probes and blows into his nose is complicated. That’s why we do it when he’s asleep.
This is also the moment when Manuela usually tries to change the dressing that secures the gastric tube and oxygen catether. Another sporty thing to do! Thank you health plan for your help with the nurse who was on the list but you turned her down!
Between 4am and 5am, he poops (yes, we’re precise now 😅).
Then, at around 5.30-6am, we take a 5-minute walk downstairs to show him the sunrise.
The first few times, it was magical to watch him contemplate the trees and birds.

Then comes the medicine and the bath, and the day begins.
Medication
Here’s the program:
05h
Esio
Colikids
06h
Prelone
Domperidone
Symbicort
12h
Domperidone
Azithromycin
16h
Symbicort
18h
Domperidone 1 mL
Vitamins (Sanyd, Noripurum, Growit, Zinco)
Neozine
21h
Spiriva
22h
Symbicort
00h
Luftal
Most of these drugs are administered via a syringe which is prepared and inserted into the catheter.
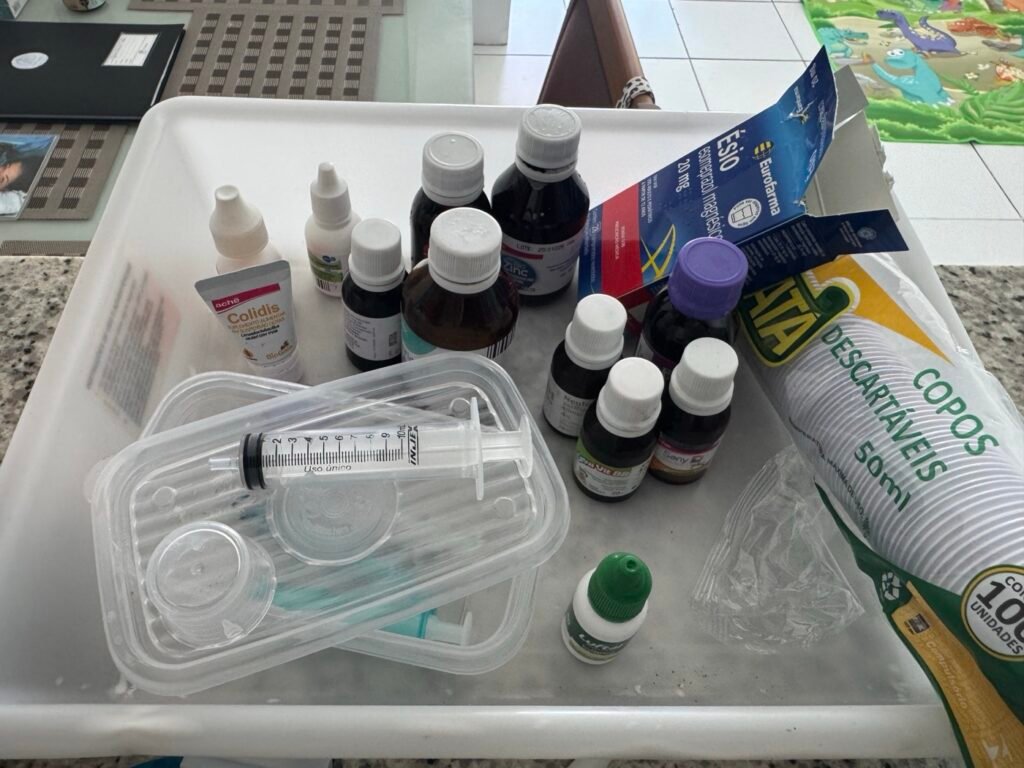
Syringes that give us a hard time because they often jam and explode!
Note that when the child cries, there’s no point in trying to inject anything – it always spills out of the tube! You learn little by little.
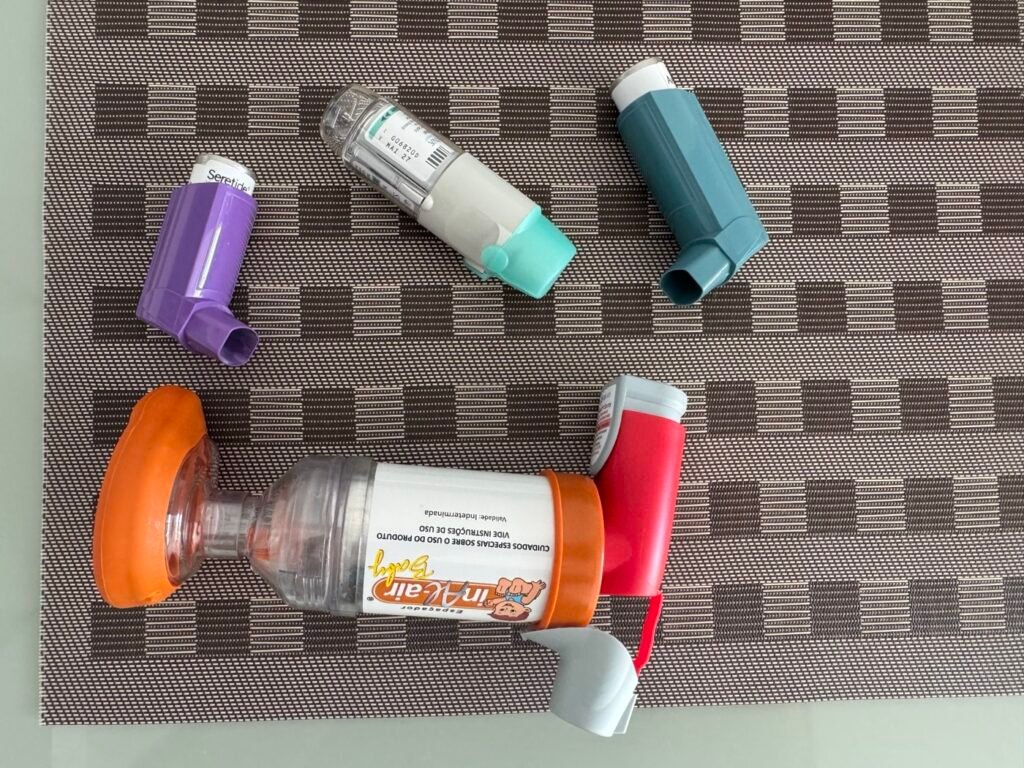
There are also aerosols, which Gabriel hates.
Feeding
Gabriel is tube-fed every three hours.
The milk descends by gravity into a small hanging flask.
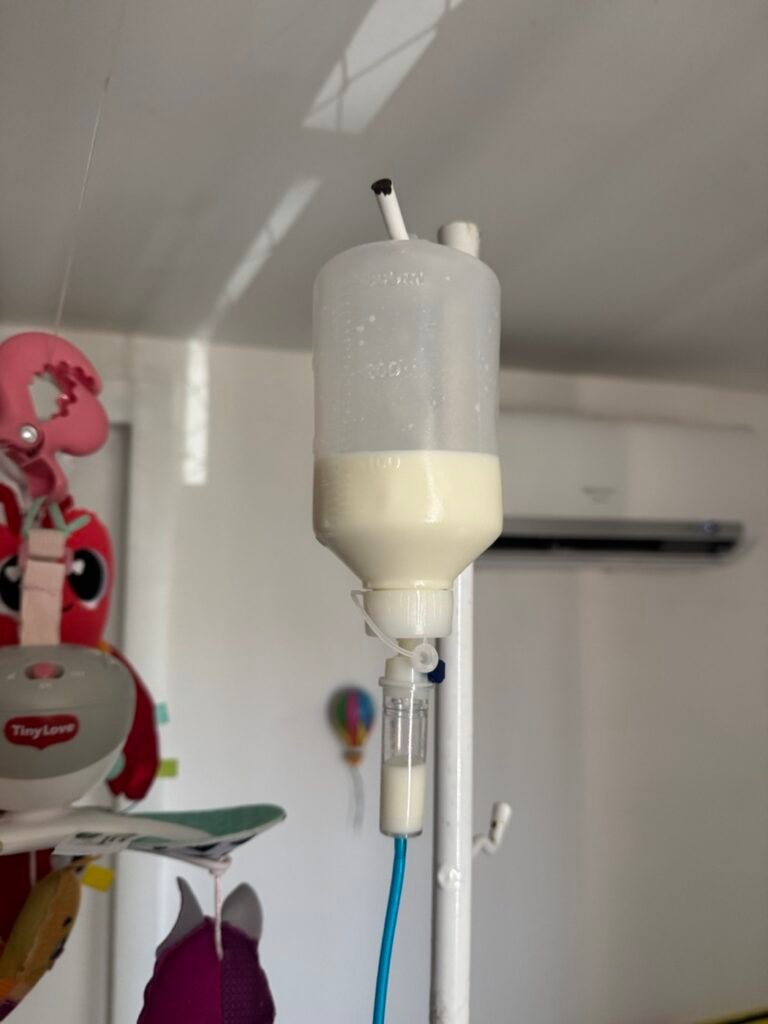
The problem: the flow is manual.
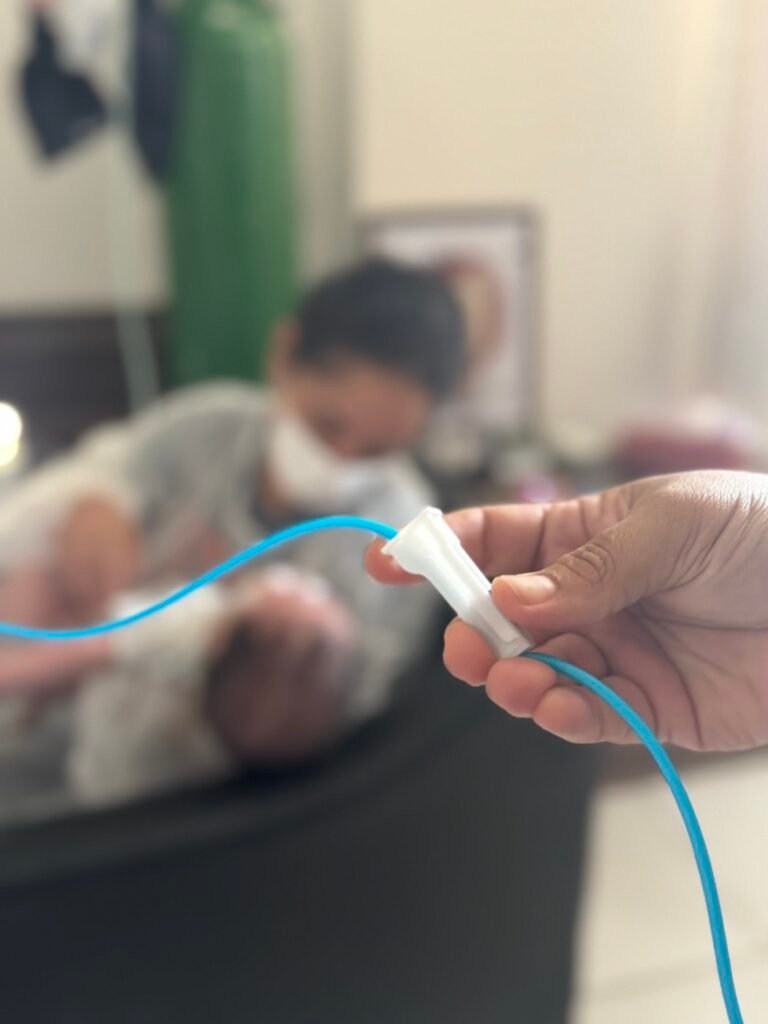
And sometimes the milk goes down too quickly, depending on her movements, her high position and her cries.
Result: Gabriel vomits, with the risk of bronchoaspiration (milk in the lungs).
Hence the need to always have someone with him. A small problem can escalate very quickly.
The pneumologist asked for an automatic regulator, but the health plan refused. (Thanksiii to one of Brazil’s richest guys for teaching us how to save money!)
Is it a health plan or a death plan?
(As JP Fanguin would say… the question is quickly answered).
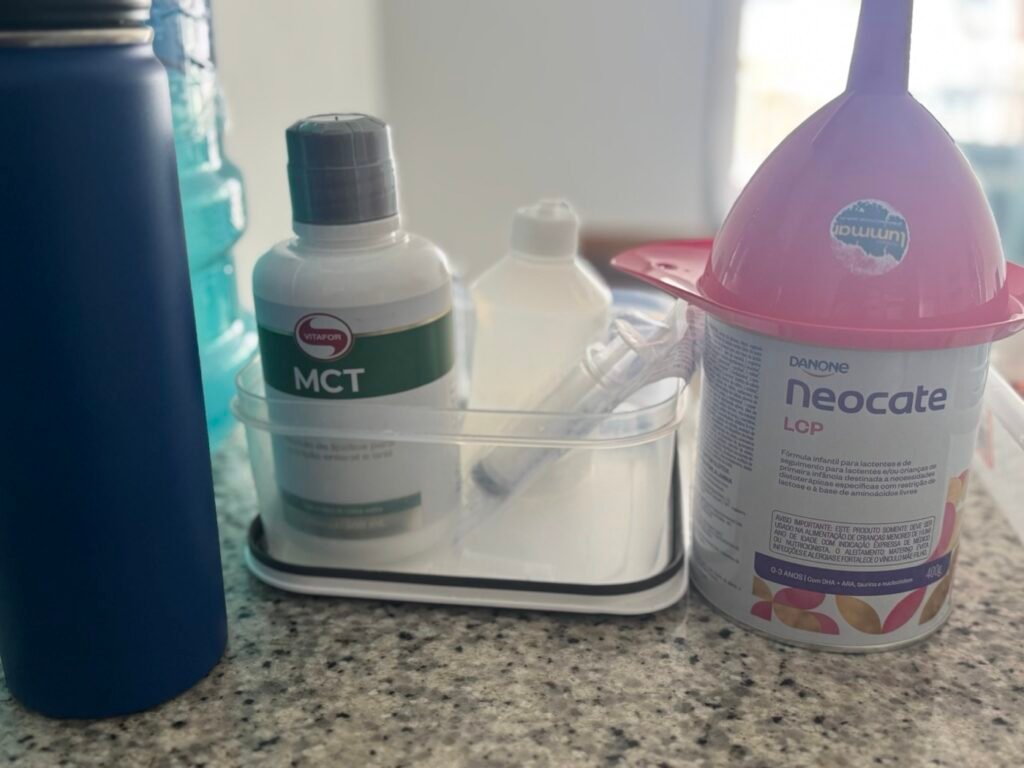
The milk is a special milk to which fat is added. It’s a good monthly budget, costing around R$2,000 a month.
He had Infratini, we switched to Neocate as he seems to be intolerant to the former.
Care and follow-up
Gabriel has, in theory, two daily sessions of respiratory physiotherapy via the PGC (health plan program).
But sometimes no one comes (usually at weekends), and no one fills in.
Complaints are made, responses are slow in coming.
He also has three sessions a week with a PGC speech therapist to relearn how to swallow.
The process may take a little longer, but we’re making progress.
The fear here is the risk of bronchoaspiration: if Gabriel breathes in milk, lung infection will be rapid and so will a return to hospital.
A possible gastrostomy (a direct opening to the stomach with a “button” on the belly) is evoked.
This would free up his nose, but we’re still hoping to avoid this solution.
Every 3 days we have an oxygen supply.
It’s a bit tricky when it comes to scheduling because they come when they want.


He was also supposed to have a pediatrician who would visit him 2x months.
We’re still waiting for him…
Well, I’m a bad tongue because we had a doctor. But a doctor doesn’t have 3 years of pediatric training.
Does it make a difference to a baby with a serious chronic illness?
(I’ve also asked the PGC and I’m still waiting).
Accommodation
We live in a condominium.
It’s typical in Brazil of large buildings surrounded by fences with guards at the entrance.
From my point of view, these kinds of spaces are a bit like “golden prisons”.
Thought to Sarko (joke)
Inside there’s everything, you can live without ever leaving.

Neighbors (who must have some pretty shitty lives compared to ours), have nothing to do but complain about us drying the sheets on the balcony or leaving shoes on the doormat.
The level of trouble in their heads! I can’t even imagine! It must be so hard to deal with…
Here, there are rules for everything.
We also can’t receive oxygen between 6 p.m. and 8 a.m., except that we don’t decide on delivery times.
We pay around R$4,500 all-in rent for an apartment chosen at the request of the hospital doctor, supposedly to facilitate PGC management.
Result: today, the PGC has written on our file that we are “too far” from everything.
(For those who know Fortaleza, we’re in Papicu)
Look for the mistake.
We don’t particularly like this place, but we’re bound by a one-year contract, and we’ll make do…
For half the price, we could have had a house where we wanted it, and now we know it was better for the PGC, according to the PGC professionals… It’s beyond comprehension!
The apartment’s not bad, a bit too small for all Gabriel’s gear, but when you’ve lived in your own home as a landlord in the country, living in a prison in the city with the noise of traffic is no joke.

Alternative care
Faced with the shortcomings of the health plan, we had to take on extra staff:
- motor kinesis (every day) to try to catch up on the developmental delay,
- a respiratory physiotherapist specialized in obliterative bronchiolitis and NIV,
- another speech therapist to speed up probe removal.
All these people do an exemplary job.
We also need an occupational therapist as soon as possible.
We have also contracted a number of specialists to give us guidance on how best to develop Gabriel.
At the same time, we sometimes take ambulances out for other examinations.
Manuela also tries to explore all possible solutions to reduce our costs via the Brazilian healthcare system, while I look at what we can do via the law to assert our rights.
I send claims almost every day to the health plan. I even have their lawyer emailing me now. I consider it a gesture of love.
Yesterday, I sent a new type of claim to the organization that manages health plans in Brazil, hoping it might help…. (Reclamation NIP à l’ANS) You need to have a BAC +5 to do it successfully. I was frankly amazed at the complexity of the thing.
In short, we spend a considerable amount of time trying to find solutions (at least half our time when we’re not sleeping or with Gabriel).
Financial reality
Between health expenses, rent, living expenses and our professional activities,
you need to generate at least R$50,000 a month to cover everything.
And unfortunately, that’s not what we earn today.
After six months of not being able to really manage our businesses :
- Manuela has almost no bookings at the moment
- As for me, I’ve left my marketing to the wayside, trying to do as little as possible for my existing customers.
And it’s a good thing I’ve got my existing customers! Thank you for continuing to trust me. You save us!
So every month, we spend more than we earn.
And we lack the time and energy to devote ourselves fully to our activities, not to mention the various interruptions caused by the arrival of a specialist and schedules that change every day, and milk, and medication etc. etc….
We hope this is temporary.
Meanwhile, the health plan congratulates itself in its response emails on its “commitment to service quality”, while refusing vital requests.
They’re real champions!
On the advice of friends and family, we’re planning to make an appeal for donations in the near future to help us get through the first six months. Personally, I don’t like asking… we’ll see.
What we remember
No, it’s not easy.
Yes, there are days when everything seems insurmountable, and jumping from a tower seems a conceivable experience.
But every time, Gabriel reminds us why we keep going.
He needs us.
I often say to myself that I was lucky to have had a good life before, to have grown up with a good education, surrounded by intelligent people, in a country that lived through the Age of Enlightenment (that makes all the difference culturally).
Then, afterwards, to have had the courage to do what I wanted with my life, and to have had so many experiences that I’d never imagined I’d be able to have.
Jim Rohn says we’re the average of the five people around us.
I wish Gabriel could have these 5 quality people to grow with.
I always believe that we are in control of our lives and that what happens to us in life is the fruit of our decisions and actions.
That’s why I feel I’m partly to blame for all this, not least because of my actions, my choices and my unspoken words.
I’d like to talk to a shrink about it more often, but that’s another cost to add. Besides, it takes time…
And during this already precious time, I don’t work.
I want to make up for this guilt by offering her the best possible future.
But it’s clearly not easy to choose which path to take when you’re in the middle of chaos.
I leave you with the only thing that gives us the strength to carry on: his smile.

